Chronic Obstructive Pulmonary Disease (C.O.P.D) encompasses chronic bronchitis (“blue bloaters“) and emphysema (“pink puffers“)
Pathophysiology: Inflammation leading to mucus hypersecretion and destruction of alveolar walls. The airway walls become weak and close (or “obstruct”) as patient tries to exhale, trapping air (including CO2) in the lungs
Risk factors:
- Smoking
- Alpha-1-antitrypsin deficiency (genetic)
- Various other (including infections such as HIV)
Diagnosis:
- Outpatient
- Pulmonary Function Tests
- Obstruction diagnosed by: FEV1/FVC < 0.7
- No bronchodilator response (<12% increase or <200 mL increase in Tidal Volume)
- Absent methacholine response
- Emphysema: Decrease in DLCO
- Chronic Bronchitis: Normal DLCO (>75% of predicted value)
- Pulmonary Function Tests
- Inpatient “Exacerbation” (if patient has known or suspected diagnosis of COPD)
- Increased dyspnea and/or cough/sputum worsening in less than 14 days (1)
Outpatient Management
- Non-Pharmacologic
- Smoking cessation
- Exercise regimen
- Immunization (Influenza and Pneumococcal)
- Supplemental Oxygen (target an SpO2 ~88-92)
- BiPAP (if CO2 retention)
- Procedures
- Lung reduction surgery (especially if emphysematous changes are worse in the upper lobes of the lung)
- Placement of one-way endobronchial valves to prevent CO2 retention
- Lung transplant
- Pharmacologic management is based on the patient’s Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification. Examples of medications provided below (2)
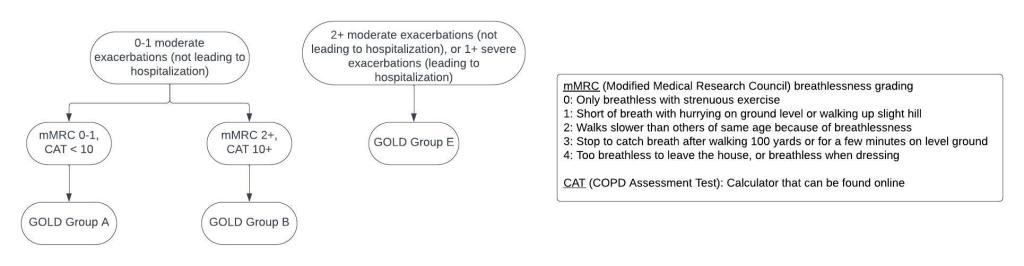
- GOLD Group A starting options:
- LAMA + as-needed SABA
- LABA + as-needed SAMA-SABA or SABA
- As-needed SAMA-SABA or SABA
- GOLD Group B starting options
- LAMA-LABA + as-needed SABA
- GOLD Group E starting options:
- Eosinophils > 300: ICS-LABA-LAMA
- Eosinophils < 300: LABA-LAMA
- SABA: Short-Acting Beta-Agonist (i.e. albuterol)
- SAMA: Short-Acting Muscarinic Antagonist (i.e., ipraptopium)
- LABA: Long-Acting Beta-Agonist (i.e. formoterol, salmeterol)
- LAMA: Long-Acting Muscarinic Antagonist (i.e. tiotropium, aclidinium)
- ICS: Inhaled corticosteroids (i.e. fluticasone, mometasone, budesonide)
- Additional therapies as below have also shown benefit in patients with COPD
- Antibiotics
- Macrolides have been shown to decrease frequency of exacerbations (usually Monday, Wednesday, Friday dosing)
- Roflumilast (Phosphodiesterase-4 Inhibitor)
- Can help prevent re-hospitalization
- Notable side effect: Diarrhea
- Biologic Agents (if asthma-COPD overlap syndrome)
- Ex. Omalizumab (anti-IgE) vs mepolizumab (anti-IL-5)
- Especially beneficial in patients with peripheral eosinophilia
Inpatient “Exacerbation” Management
- Investigate underlying cause of exacerbation
- Chest X-Ray: to rule out alternative diagnosis
- Respiratory viral panel
- CBC: Assess for polycythemia, anemia, or leukocytosis
- EKG: to look for underlying ischemia
- Consider CTA if concern for PE
- Acute Respiratory Failure
- Supplemental oxygen
- Non-invasive ventilation/bilevel positive airway pressure (BiPAP) if patient has acute CO2 retention or significant respiratory distress
- Intubation if necessary
- Obstruction
- Continue home long-acting inhalers
- Start combination SABA/SAMA nebulizer scheduled q4hours-q6hours
- Inflammation
- Steroids
- Typically start with IV methylprednisolone on day 1 (40-120 mg x1 dose)
- Change to PO prednisone 40 mg qday on the second day (course of 5-10 days)
- Antibiotics
- Controversial, typically reserved for patients who have increase in the purulence of their sputum as well as either increased dyspnea or increase in the volume of their sputum (2)
- Azithromycin, doxycyline, or levofloxacin for anti-inflammatory effects as well as to cover atypical pathogens for a course of 5-7 days
- Steroids
References
- Celli BR, Fabbri LM, Aaron SD, et al. An Updated Definition and Severity Classification of Chronic Obstructive Pulmonary Disease Exacerbations: The Rome Proposal. Am J Respir Crit Care Med 2021; 204(11): 1251-8.
- Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary. Eur Respir J. 2023 Apr 1;61(4):2300239. doi: 10.1183/13993003.00239-2023.

