Angina (Typical = 3/3 symptoms, Atypical = 2/3)
- Substernal chest pain
- Pain exacerbated by exertion
- Pain relieved with rest or nitroglycerin (or both)
Management
Non-ST-Elevation ACS (includes Unstable Angina and NSTEMI)
- HEART (History, EKG, Age, Risk Factors, Troponin) score
- Risk stratifies patients who present with chest pain as to their risk of major adverse cardiovascular events (MACE). This score can help guide decisions in terms of decision to hospitalize and at what level of care
- TIMI (Thrombolysis in Myocardial Infarction), GRACE (Global Registry of Acute Coronary Events) scores
- Helps to guide early-invasive (coronary angiogram within 24-48 hours) vs. ischemia-driven (medical management with angiogram if patients have recurring symptoms and/or positive stress test) in patients with suspected ACS. These scores can also help predict major adverse cardiovascular events, though they appear to be inferior to the HEART score in this regard
- Pharmacologic Management
- Aspirin 324 mg load followed by 81 mg daily
- Second antiplatelet agent (at Cardiology’s discretion)
- Clopidogrel 300-600 mg load followed by 75 mg daily
- Ticagrelor 180 mg load followed by 90 mg BID
- Note that self-limiting shortness of breath may be an observed side effect
- Prasugrel 60 mg load followed by 10mg daily
- Heparin continuous infusion
- Nitroglycerin administration
- Sublingual vs PO isosorbide mononitrate (once daily dosing) vs PO isosorbide dinitrate (q8hours dosing) vs IV continuous nitroglycerin
- Contraindicated in right-sided MI (as these patients are preload-sensitive and nitroglycerin will decrease preload) or in a patient using sildenafil or tadalafil
- Sublingual vs PO isosorbide mononitrate (once daily dosing) vs PO isosorbide dinitrate (q8hours dosing) vs IV continuous nitroglycerin
- Beta-Blocker
- Typically initiated within 24 hours
- Contraindications: Bradycardia, heart failure signs/symptoms, severe asthma
- Typically initiated within 24 hours
- ACE-Inhibitor/Angiotensin-Receptor Blocker
- Typically lisinopril or losartan initiated within 24 hours if blood pressure allows to prevent cardiac remodeling
- Statin
- Typically Atorvastatin 40-80mg daily
ST-Elevation Myocardial Infarction

- ST-elevation Equivalents
- Hyperacute T-waves, De Winter Syndrome, Wellen’s Sign A and B, “Shark fin”
- Pharmacologically managed the same as Unstable Angina or an NSTEMI
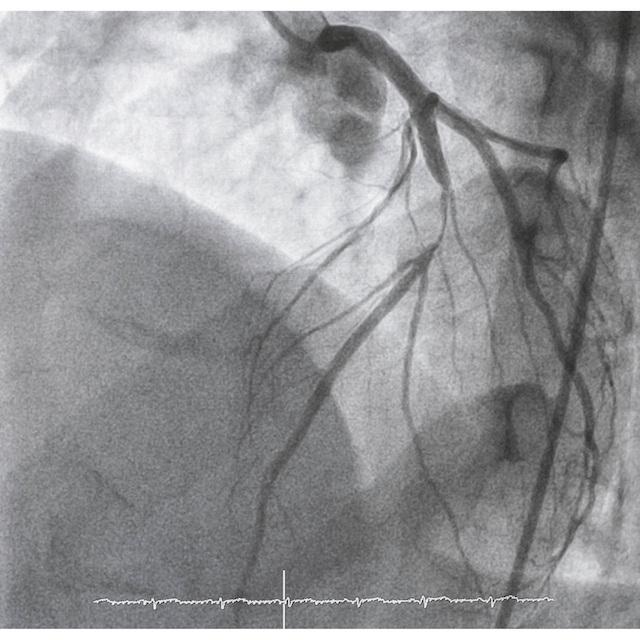
- Coronary Angiogram: Standard of care: door-to-balloon time less than 90 minutes
- Bare Metal Stent: Must be on dual-antiplatelet therapy (DAPT) for 1 month to prevent in-stent thrombosis. Higher risk of in-stent stenosis than drug-eluting stents.
- Drug-Eluting Stent (usually everolimus-eluting): The eluted drug prevents in-stent stenosis but also delays epithelialization of the stent, and for this reason patients must generally receive DAPT for at least 6-12 months to prevent in-stent thrombosis
- Thrombolysis
- Fibrinolytics indicated if there is no access to a catheterization lab
- Requirements:
- Symptomatic
- Symptomatic for < 12 hours
- Persistent ST-elevations
- Contraindications: Many, but mostly summarized to any increased risk of bleeding (low platelets, intracranial malignancy, history of aortic aneurysms, history of large GI bleeds, recent surgeries, etc.)
- After fibrinolysis, transfer to center with cardiac catheterization capabilities
- Requirements:
- Fibrinolytics indicated if there is no access to a catheterization lab
Coronary Artery Bypass Graft (CABG) indications
- 3-vessel disease
- 2-vessel disease including proximal left anterior descending artery (or if diabetic)
- Left main artery disease